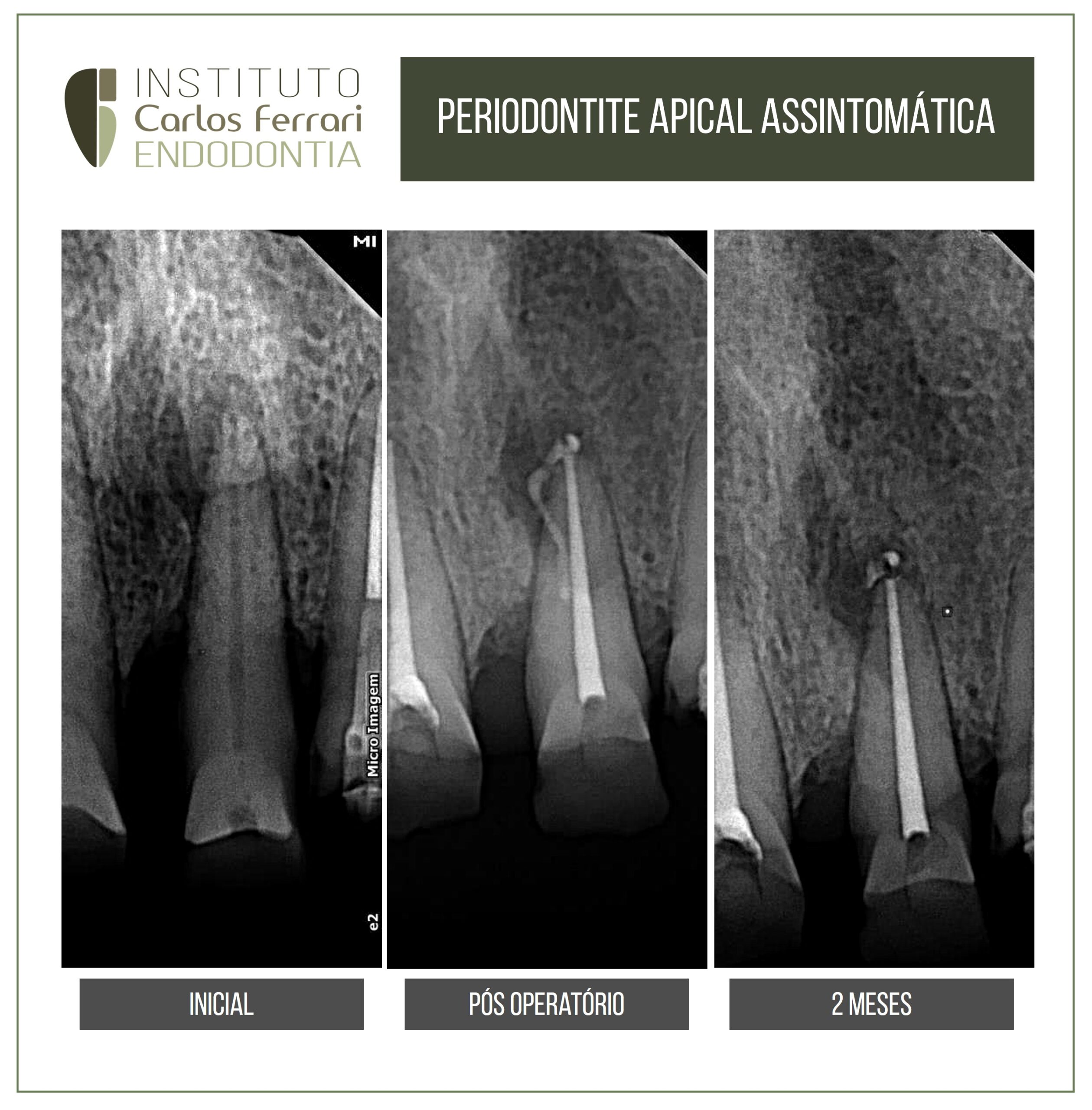
Asymptomatic apical periodontitis. Case of asymptomatic apical periodontitis, with obturation of the lateral canal, probable cause of the inflammatory process origin of the radiolucent image. Proservation of 2 months showing the resorption of the cement and repair in progress.Case of Fernanda Santiago, student of specialization in endodontics at HPG Brasília.
https://ferrariendodontia.com.br/livro-endodontia-ricardo/
https://www.youtube.com/watch?v=QMLd1CcjsO0&t=1130s
Morphological evaluation of the nasopalatine canal and its variations analyzed by means of cone-beam CT images of
Fernando Mathias Teixeira Velho; Danielle Freire; Rodrigo Montezano; Nádia Assein Arus; Heraldo Luis Dias da Silveira; Mariana
Boessio Vizzotto; Heloisa Emilia Dias da Silveira - UFRGS
Introduction: The need for the anatomical identification of the nasopalatal canal and its variations has grown due to the increase in indications of dental implant placement, which generate higher aesthetic expectations backed by the success of the surgical technique. Multiplanar Cone-Beam Computed Tomography (CBCT) images are considered the gold standard for detecting morphological variations in vivo. Objective: To investigate the anatomical variations found in the nasopalatal canal by means of CBCT scans, relating them to gender, number of canals and presence of Stenson foramina. Methodology: A cross-sectional observational study was performed where 3 calibrated observers analyzed 1026 CBCT scans investigating nasopalatine canal amorphology and its variations. By means of the chi-square test (χ2) the correlation between the variables gender, amount of canals and Stenson foramina was evaluated (significance of 0.5%). Results: After the exclusion criteria were applied, 965 exams continued to be evaluated, of these 540 were female and 425 were male, with a mean age of 49.98 years (SD= ±15.88). The descriptive analysis of the variable number of canals showed that 71% of the patients presented a single canal (45% in males and 55% in females). The variable number of Stenson foramina showed that61% of the patients presented a single foramina (46% in men and 54% in women). The chi-square test (χ2) showed no significant difference between men and women for number of canals and presence of Stenson's foramina (p=0.261 and 0.438, respectively).
Conclusion: The results found in this study show that there is no difference between genders regarding the number of occurrences of nasopalatine canal and Stenson's foramina. Key Words: Maxilla; X-ray computed tomography; Anatomical variation
Excerpt from the chapter: Radiology Applied to Endodontics. Ferrari et al, in Machado R. Endodontia. Bases Biológicase técnicas. Ed. Gen, 2002.
Overlapping images in Endodontics
Some anatomical structures present radiolucent radiographic images that, depending on their position, can be confused with periapical bone rarefaction of endodontic origin. Variations in X-ray beam angulation (Clark technique), together with previous information obtained through anamnesis and clinical examination, are fundamental for the differential diagnosis.
In the maxilla, the structures capable of producing such effect are the palatine canal and foramen, which can have their image superimposed on the apexes of the upper central incisors, especially in radiographs with distroradial incidence. Another anatomical structure frequently confused with periapical lesions in premolars and especially in maxillary molars is the maxillary sinus (Figure 6.20). Its anatomical and morphological heterogeneity can produce images similar to periapical lesions that can confuse even experienced clinicians. Also in the maxilla, the periodontal ligament adjacent to the molar roots can simulate the presence of root fractures and additional canals (Figure 6.21).
In the mandible, the anatomical structures that most cause doubts in the interpretation of radiographic exams performed by different techniques are the mandibular canal - which overlaps the root apices of the molars - and the mental foramen - which can mimic a periapical lesion in premolars (Figure 6.22).
Non-endodontic pathologies with periapical radiographic manifestations
Periapical pathologies or changes not caused by pulpoperirradicular involvement may present images often confused as such. A thorough examination of the patient, initially considering the initial complaint, the case history and the results of a thorough clinical examination can in most cases provide data that allow a correct diagnosis. The absence of signs or symptoms and normal responses to vitality tests, percussion and palpation in all teeth adjacent to the lesion can already constitute a substantial indication of its non-endodontic origin.
Radiographic interpretation must be performed with attention and rigor, following specific and objective criteria, among which are: number of lesions, location, radiolucency, border characteristics, internal structures, and effects on adjacent structures and teeth.31 Such questions, when analyzed in order, facilitate the determination of diagnostic hypotheses.
The pathologies and changes of non-endodontic origin most commonly misdiagnosed as such are described below, according to their radiolucency.
Radiopaque
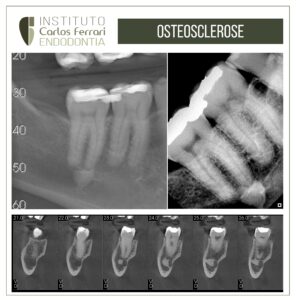
-Idiopathic osteosclerosis: a single image, usually present in the periapical region of the lower posterior teeth, with variable radiopacity, irregular borders and absence of cortical bone (Figure 6.26). It has no known etiology and requires no treatment, being frequently confused with condensing osteitis, caused by a chronic inflammatory process of endodontic origin
-Mandibular torus: external bony formations located on the mandibular lingual surface can produce radiopaque images on periapical examination with variable number and rounded shape, often overlapping the periapical region of the lower teeth (Figure 6.27). The clinical examination can confirm the suspicion by observing such formations through intraoral inspection.
Mixed
Cemento-osseous dysplasias: idiopathic lesions in which there is replacement of bone tissue by fibrous tissue. They present a mixed image, being more radiolucent in the first phase, becoming mixed and then radiopaque after maturation. They are more common in black patients, females and in adulthood, self-limiting and frequently diagnosed by means of routine radiographs. However, because they are located in the periapical region, their presence is commonly associated with unnecessary endodontic treatment. Cemento-osseous dysplasias are subdivided into periapical cemento-osseous dysplasia, more localized in only one region (often in the anteroinferior teeth), and florid cemento-osseous dysplasia, with multiple images spread throughout the arch (Figure 6.28)
-Other pathologies with mixed radiographic images that can mimic lesions of endodontic origin are odontomas and benign cementoblastoma.
Radiolucent
-Cysts: Several cysts of non-endodontic origin are capable of producing images similar to those originating from pulpo-perirradicular involvement, such as: the lateral periodontal cyst (usually located in the region of lower premolars); the dentigerous cyst (more frequent in lower molars) (Figure 6.29), the keratocyst (common in the mandible) (Figure 6.30), the traumatic bone cyst and the nasopalatine cyst (frequent in maxillary anterior teeth)
-Other pathologies capable of mimicking periradicular lesions are: adenomatoid odontogenic tumor (most common among lateral incisors and maxillary canines), giant cell lesion, intraosseous fibromas and lipomas, ameloblastoma, and malignant tumors. An anatomical alteration that produces a radiolucent image in the mandibular angle region, but which can rarely appear in the periapical region, is Stafne's bone defect.
Asymptomatic apical periodontitis