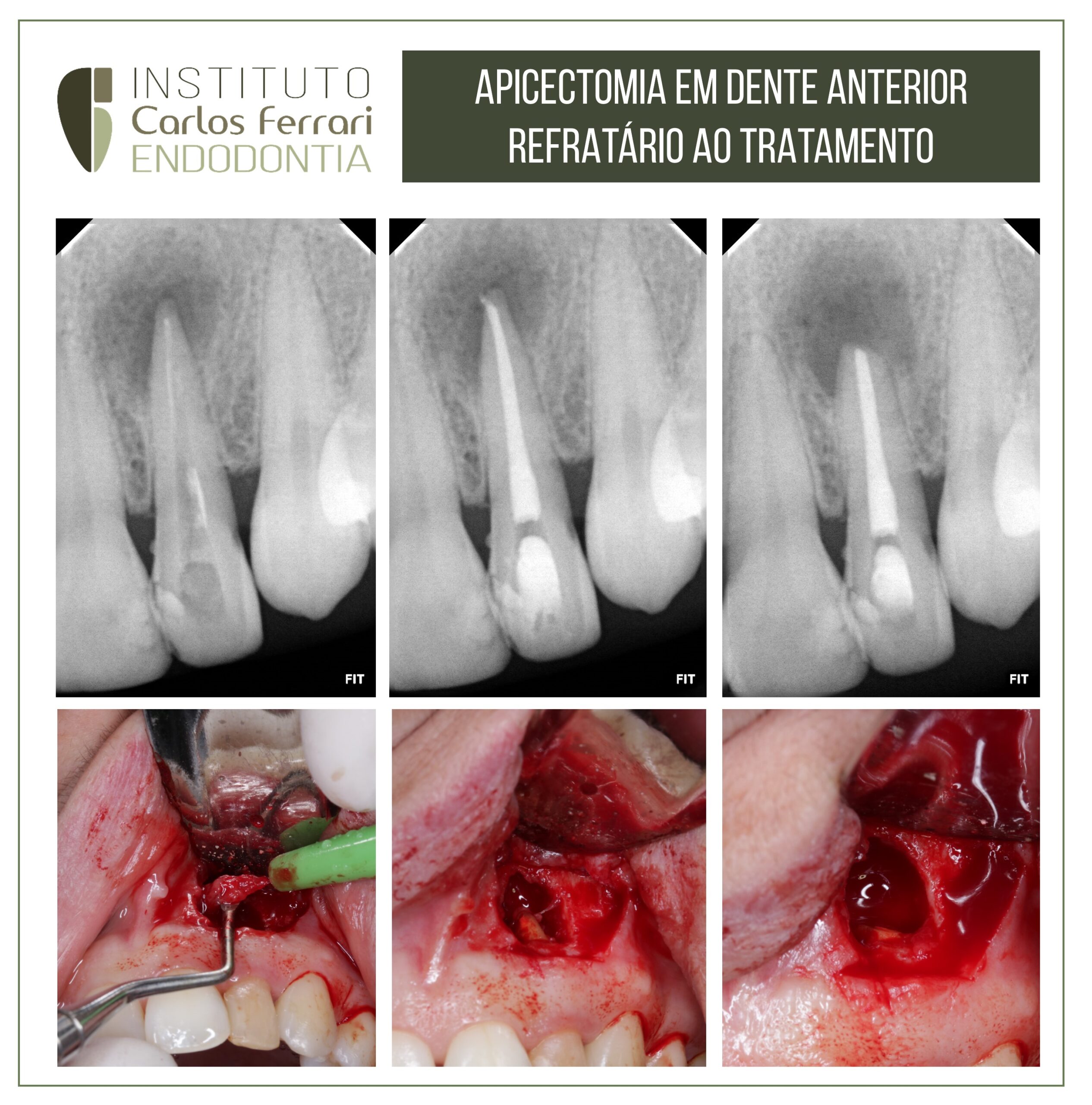
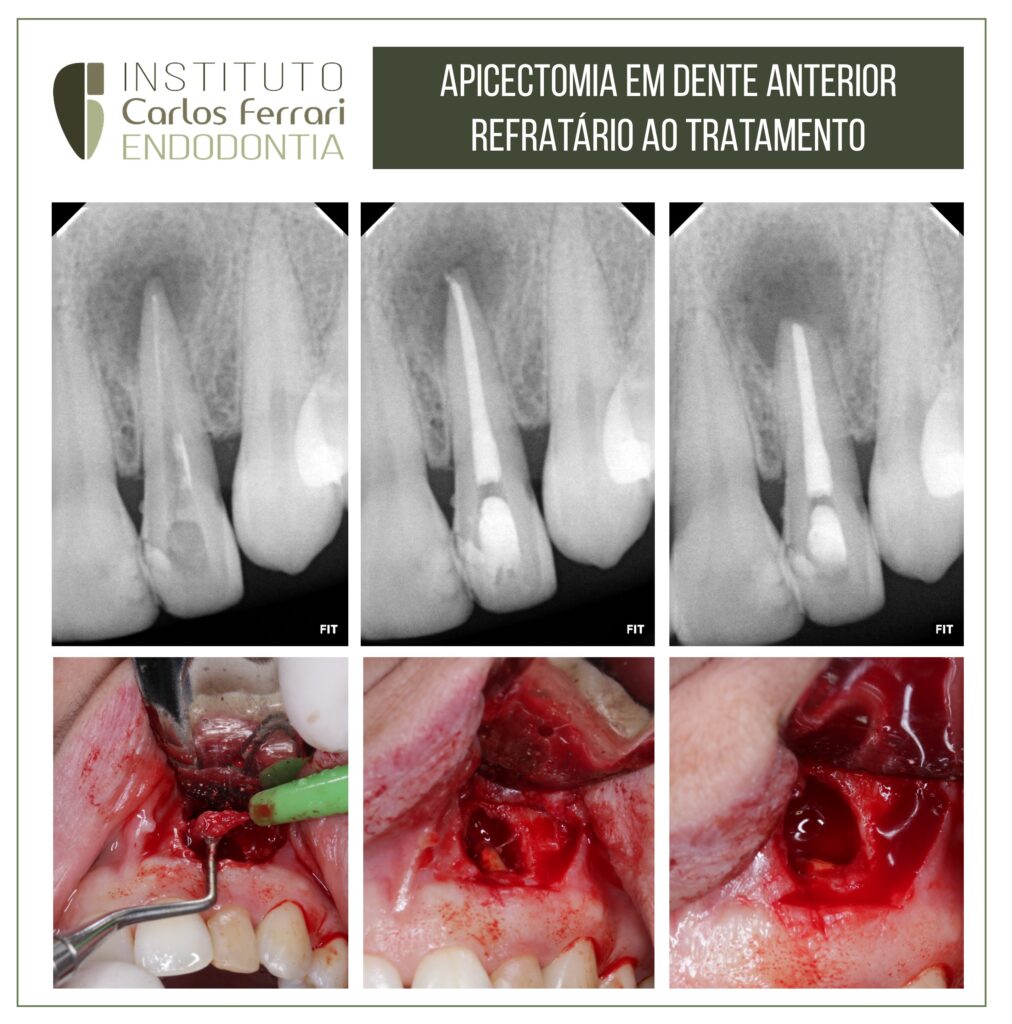
Endodontic treatment failure. Apicectomy in paraendodontic surgery.
The patient underwent endodontic treatment of tooth 22 with successive changes of medication, without remission of the fistula.
Case conducted by Joice Gandini and Igor Fajan, students specializing in endodontics at APCD Bragança Paulista.
Paraendodontic surgery and fixed prosthesis. In: Marchetti et al. Paraendodontic surgery: clinical case report. RSBO v. 5, n. 2, 2008
The paraendodontium comprises the periapical region, the periradicular zone and bordering regions, to which endodontic complications may extend.
It is known that endodontic treatment should provide complete obliteration of the entire root canal system. The establishment of an adequate sealing aims to prevent microorganisms and/or endotoxins from reaching the apical and periapical tissues
In situations where failure is observed in conventional endodontic therapy after the tooth is restored, with intracanal core or even as a support for fixed prosthesis, the surgical procedure is indicated. Also in cases of persistent periapical lesions or even with cystic characteristics, calcified root canals with periapical lesions where it is impossible to access via pulp chamber, fractured instruments, apical perforations and steps, the way to circumvent and solve the problem is the indication of paraendodontic surgery.
According to Berbert et al. (apud Bernabé and Holland, the correct terminology for this procedure is paraendodontic surgery, because it covers all types of surgical interventions related to endodontics. For a long time, endodontic surgery was the exclusive domain of the oral and maxillofacial surgeon.
Recently it started to be approached by the endodontist, who is the most indicated professional to perform it, because he knows in detail the anatomy of the root and canal and its consequent implications in a periapical process. The constant evolution of endodontic techniques makes root canal treatments reach high levels of success, but these procedures are subject to failures and accidents in their execution.
In the event of endodontic treatment failure, retreatment may be chosen. But in cases where this is not possible, the paraendodontic surgery is an excellent alternative for solving problems not solved by conventional treatments.
The paraendodontic surgery is a set of procedures aimed at resolving complications arising from a root canal treatment or its failure. It is indicated when it is not possible to have access to the canal system in teeth with periapical lesion, due to calcified canals or those obstructed by fractured instruments, as well as in cases where there is extravasated filling material, failure of conventional treatment and impossibility of retreatment, apical perforations, teeth with core or those with fixed prosthesis.
Contraindications may be local or general. Local contraindications occur when it is possible to treat or retreat the canal and when there is impossibility of surgical access, insufficient periodontal support, pathological processes in acute phase and risk of injury to anatomical structures. Some of these contraindications can be minimized with operator experience. The general contraindications include the patient's precarious general state of health and the degree of systemic involvement.
The most commonly used surgical modalities are periapical curettage, apicectomy, apicectomy with retrograde obturation, apicectomy with instrumentation and obturation of the root canal viaretrograde and obturation of the root canal simultaneous to surgery [10]. Periapical curettage is a surgical procedure that has the purpose of removing pathological tissue in a lesion at the apical level of a tooth or foreign bodies in the periapical region [5, 10]. In some situations, in case of pulp necrosis and periradicular injury, there is formation of a periapical biofilm that is difficult to eliminate by conventional endodontic procedures and medications. This layer is colonized by bacteria that can perpetuate the peri-radicular injury. Thus, periapical curettage should be performed to remove the microbial biofilm. According to Leal et al, curettage should always be accompanied by apical plasty, i.e., careful smoothing of the root apex. This procedure is necessary because the cementum covering the apical portion of the root is resorbed.
Apicectomy is the surgical removal of the apical portion of a tooth. It is indicated in numerous clinical situations, such as periapical lesions persistent to conventional treatment, perforations, fractured instruments, removal of apical deltas, presence of external resorption, among others.
The apicectomy associated with retrograde obturation consists of removing the apical portion of a tooth, preparing a cavity in the final portion of the root remnant, and obturating this space with adequate material. In cases where there is a need for disinfection and sanitation of the root canal, retroinstrumentation and subsequent retroobturation are performed.
The obturation of the canal simultaneous to surgery consists in the periapical curettage with apicectomy of a tooth, followed by conventional obturation of the canal system during surgery. It is indicated to solve cases of extensive chronic periapical lesions in which the canal is well instrumented and numerous exchanges of calcium hydroxide have been performed, but there is the presence of inflammatory exudate preventing the conclusion of the case.
Several authors have reported cases of para-endodontic surgery in the literature, showing the diversity of clinical situations and techniques used. Mariano and Messora performed apicectomy in teeth with extensive periapical bone loss and, as there was absence of bone support for flap support, they used collagen membrane to guide tissue regeneration. In the radiographic proservation of the case for four years, they observed complete reduction of the radiolucent area with good bone repair.
Rosa et al. described a case of apicectomy associated with retrograde obturation with MTA in a tooth with fixed prosthesis with periapical lesion, obtaining bone tissue neoformation in a period of seven months.
The choice of the retroobturator material is of fundamental importance for the success of the paraendodontic surgery. The ideal characteristics of the retroobturator material must be: non-toxic, non-mutagenic, biocompatible and insoluble. In addition, it must adhere to the tooth structure and maintain its sealing capacity for a long period of time, besides being easy to manipulate, radiopaque, dimensional stable, and unaffected by humidity.
Endodontic treatment failure