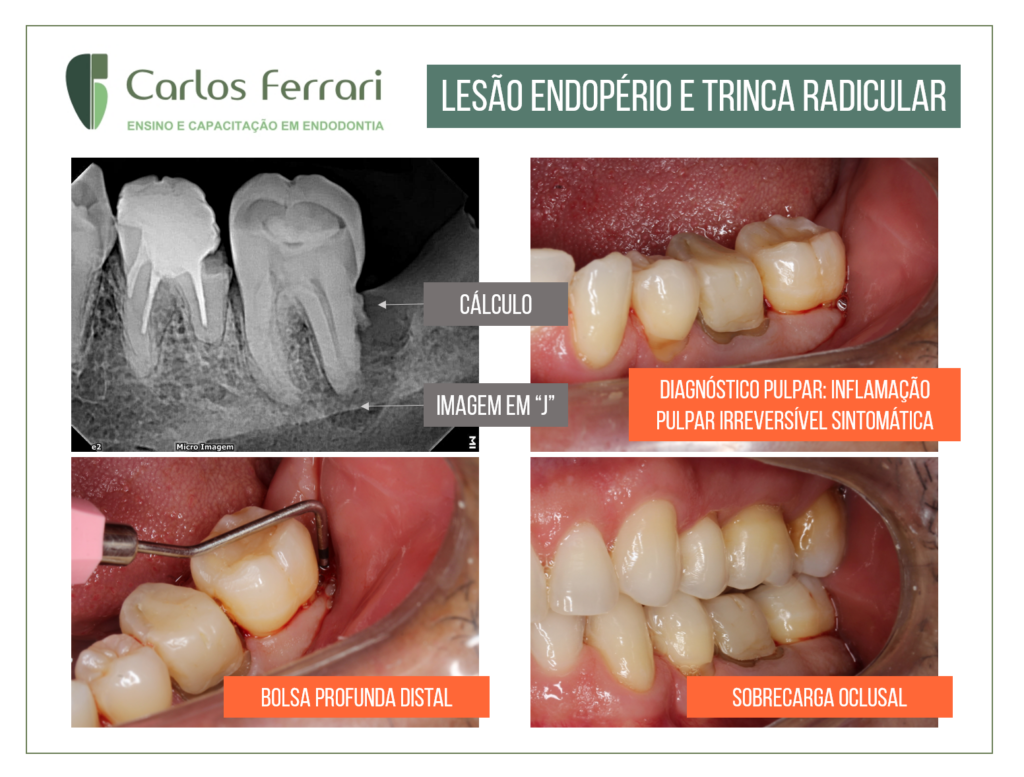
Lesion endoperio. Inferior molar with pulpitis and a suspected crack in the distal root.
Patient came to the office complaining of pain on hot and cold, characteristic of pulpitis. The clinical examination revealed as causal tooth, tooth 37, and deep pocket in the distal region. As aggravating factor, the patient had brachi pattern, with unbalanced occlusion on the tooth. Radiographic examination revealed calculus and a J-shaped image on the distal root, suggesting a crack. After pulpectomy, the patient was investigated using a microscope and methylene blue solution for cracks in the pulp chamber, and no evidence was found. Intracanal bioceramic medication was then placed (Bio C Temp), and the leakage through the probable crack was observed. After 1 week, there was partial resorption of the extravasated medication.
After 1 month, the filling was done, and the patient was instructed to see a periodontist and return for follow-up.
Lesion endoperio In: Oliveira et al. Clinical surgical treatment of endoperiodontal lesions. Case report.
Introduction:
The interrelationships between pulpal and periodontal diseases occur primarily due to the intimate anatomical and vascular connections between the pulp and periodontium; these interrelationships have traditionally been demonstrated using radiographic, histological and clinical criteria. Some studies suggest that the two diseases may have etiological influences on each other's progression.
The main communication pathways between the two tissue types are the apical foramen, the lateral and accessory canals, and the dentinal tubules (Cohen and Hargreaves, 2011). Endodontic-periodontal diseases often present challenges to the clinician regarding their diagnosis, treatment, and prognostic evaluation. For differential diagnosis and treatment purposes, so-called "endo-perio lesions" are best classified as primary endodontic diseases, primary periodontal diseases, and combined diseases. Combined diseases include: primary endodontic disease with secondary periodontal involvement, primary periodontal disease with secondary endodontic involvement, and true combined diseases (Lopes and Siqueira, 2015).
Primary periodontal disease with secondary endodontic involvement and combined endo-perio diseases require both endodontic and periodontal considerations. The prognosis of primary periodontal disease with secondary endodontic involvement and true combined diseases depends primarily on the severity of the periodontal disease and the response of the periodontal tissues to treatment. True combined diseases often have a poor prognosis. Generally, adequate endodontic treatment will result in healing of lesions of pulpal origin. The prognosis of combined diseases depends primarily on the success of periodontal therapy (Walton and Torabinejad, 2010).
The symptoms of marginal periodontitis, such as the presence of deep purulent periodontal pockets, gingival edema, tooth mobility, bone resorption evidenced radiographically, may be such as symptoms triggered by an endodontic cause. Sometimes, although more rarely, a radiographic image of periapical radiolucency may be a consequence of pulpal mortification and infections induced by the evolution of marginal periodontitis (Jivoinovici et al., 2017).
A broad spectrum of different therapeutic options and/or therapeutic sequences including endodontic and periodontal treatment with non-surgical and/or surgical procedures with or without local or systemic antibiotics has been described in case reports and clinical studies (Schmidt et al., 2014).
https://www.youtube.com/watch?v=6Z3H1HrJhP8&t=78s
https://ferrariendodontia.com.br/inflamacao-pulpar-reversivel/
Injury endoperio