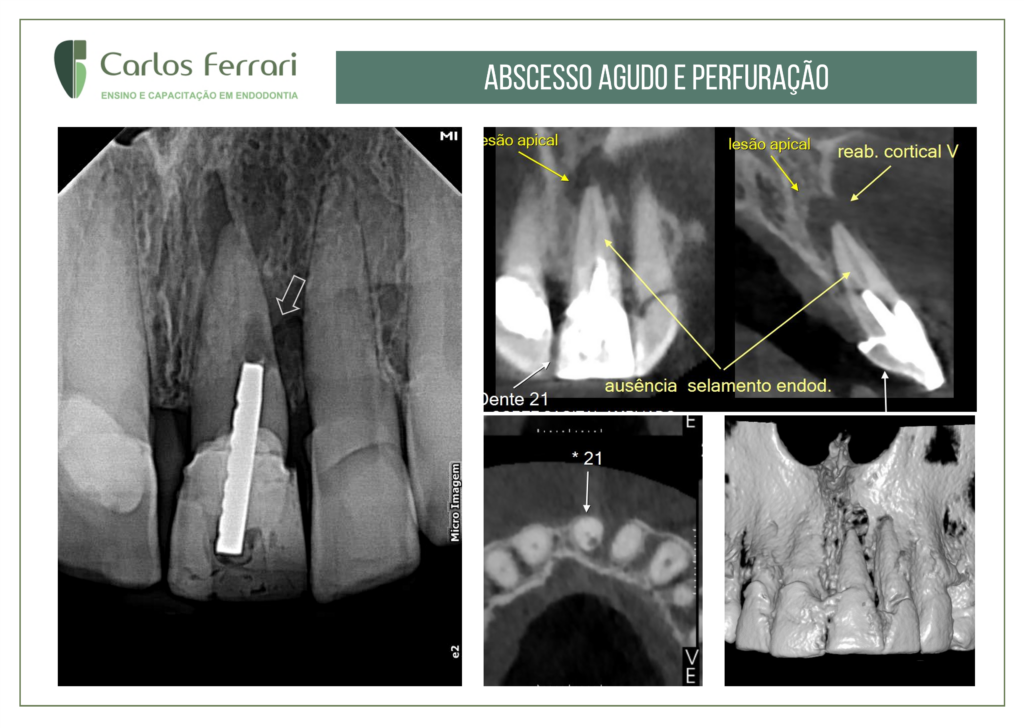
Perfuração radicular. Paciente especial com dor intensa e a indicação por parte do colega, de resolução em consulta única, sem retirada da prótese e intervenção convencional.
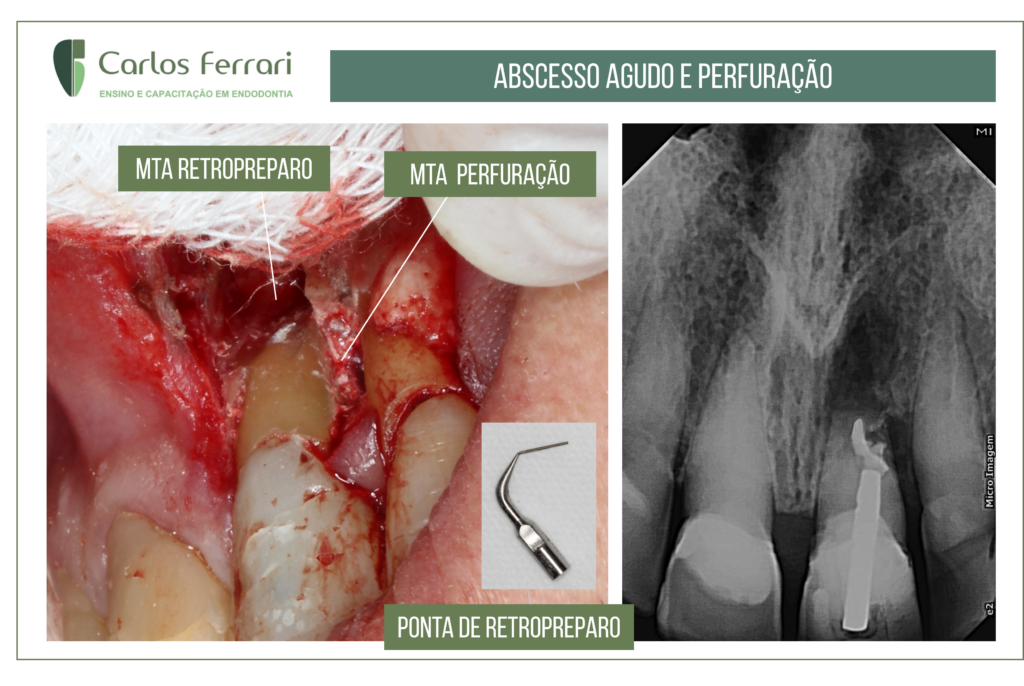
No exame clínico, edema na região gengival vestibular do dente 21. O exame radiográfico e a tomografia revelaram imagem radiolúcida periapical e na região palatina/distal, por perfuração relacionada ao retentor. Optou-se então pela resolução cirúrgica, com apicectomia e retropreparo do remanescente apical e preparo com ultrassom na região da perfuração.
Obturou-se ambos com MTA. Observou-se após 2 semanas, remissão de sinais e sintomas e o paciente foi indicado para proservação.
Dra. Vanessa Pessoti: angelus.com.br:
Durante o tratamento endodôntico, é importante considerar não apenas o resultado, mas também as possíveis complicações que podem ocorrer durante o tratamento procedimento — dentre elas, está a perfuração radicular. Por isso, é recomendado a todos os dentistas saber suspeitar, diagnosticar e tratar a perfuração radicular.
Para nos responder as principais dúvidas sobre o tema, convidamos a Profª. Drª. Vanessa Pessotti (CRO: ES 2069), dentista especializada em Endodontia. Confira, a seguir, a entrevista!
Quais os fatores podem levar a uma perfuração radicular?
A perfuração radicular está diretamente relacionada aos tratamentos endodônticos, sendo considerada principalmente uma complicação desses procedimentos — ou seja, é uma consequência iatrogênica.
Isso não significa, no entanto, que ela não possa ser evitada: a perfuração radicular está relacionada, especialmente, à não observância das particularidades anatômicas dos diferentes grupos dentais. As fases mais críticas são durante a realização do acesso coronário e durante a formatação do sistema de canais radiculares.
Alguns fatores (anatômicos e extra-anatômicos) estão relacionados a um risco aumentado de perfurações radiculares. São eles:
- morfologia irregular dos canais radiculares;
- canais calcificados;
- dilaceração radicular;
- erro durante o acesso da câmara pulpar;
- desgaste excessivo das paredes dos canais radiculares;
- preparo inadequado para colocação de pinos intrarradiculares.
Qual é a melhor forma de diagnóstico?
O primeiro passo do diagnóstico é o exame clínico e a observação das perfurações radiculares via microscópio operatório. O diagnóstico definitivo, no entanto, depende de exames de imagem, que devem ser escolhidos criteriosamente.
A radiografia periapical possui, na perfuração radicular, uma capacidade limitada: como ela oferece uma imagem bidimensional, ocorre uma sobreposição de estruturas, principalmente se a perfuração acontecer no sentido vestíbulo-lingual.
Por isso, os exames mais indicados para o diagnóstico são aqueles que permitem uma visualização tridimensional. De acordo com a Drª. Vanessa, o mais indicado é a tomografia computadorizada Cone Beam de alta resolução, que informa com maior precisão a localização das perfurações radiculares.
As perfurações radiculares possuem alguma classificação?
Sim. As classificações mais utilizadas são:
- quanto ao tamanho: pequenas ou grandes;
- quanto à localização: perfurações coronais, perfurações na zona da crista óssea ou perfurações apicais;
- quanto ao tempo transcorrido após a perfuração: “imediatas” ou “tardias”.
De acordo com a classificação, como será o prognóstico?
Segundo nossa entrevistada, conseguimos metrificar o prognóstico de acordo com algumas características das classificações (Fuss and Trope, 1996; Thesis and Fuss, 2006). Dividimos o prognóstico entre “bom” e “questionável”. Confira as características de cada um a seguir.
Sinais de bom prognóstico
- perfuração feita sob um meio asséptico e tratada imediatamente ou em curto prazo;
- perfurações de pequena dimensão;
- perfurações coronais;
- perfurações apicais (na maior parte dos casos).
Sinais de prognóstico questionável
- perfurações na zona da crista óssea;
- perfurações de grande amplitude.
Como será o tratamento das perfurações radiculares “imediatas” e “tardias”?
Como é de se esperar, as perfurações imediatas possuem tratamento diferenciado das tardias — visto que conseguem ser diagnosticadas em cenário intraoperatório e necessitam de uma intervenção mais rápida.
Nas perfurações imediatas, a Drª. Vanessa recomenda, em sessão única, fazer a desinfecção com Hipoclorito de Sódio a 2,5%; em seguida, realizar o selamento com um material biocerâmico reparador e forramento com ionômero. Se houver indicação, finalizar com a restauração de resina ou cimentação de pino.
Nas tardias, no entanto, o tratamento é realizado em duas sessões. Na primeira sessão, devemos fazer a limpeza e descontaminação da perfuração, remoção do tecido de granulação, e irrigação com Hipoclorito de Sódio a 2,5%. Em seguida, devemos prosseguir com a terapia fotodinâmica (laser de baixa intensidade) e colocar um curativo de Hidróxido de Cálcio por 15 dias.
Na segunda sessão, inicia-se com a remoção do curativo de Hidróxido de Cálcio e uma nova desinfecção. Logo, deve ser feito o selamento com um material biocerâmico reparador, seguido de forramento com ionômero e, se indicado, a finalização com a restauração de resina ou cimentação de pino.
Qual o benefício dos cimentos biocerâmicos nos casos de perfurações radiculares?
Nossa entrevistada frisa que os cimentos biocerâmicos aumentam a resistência radicular e são bem tolerados pelos tecidos. Além disso, eles apresentam a capacidade de induzir uma interação com os tecidos e a dentina, estimulando a formação da hidroxiapatita, promovendo assim, a regeneração tecidual.
Para melhores resultados, contar com produtos de qualidade é fundamental. Esse é o foco principal da Angelus, empresa que busca, dia após dia, inovar com os melhores materiais do mercado.