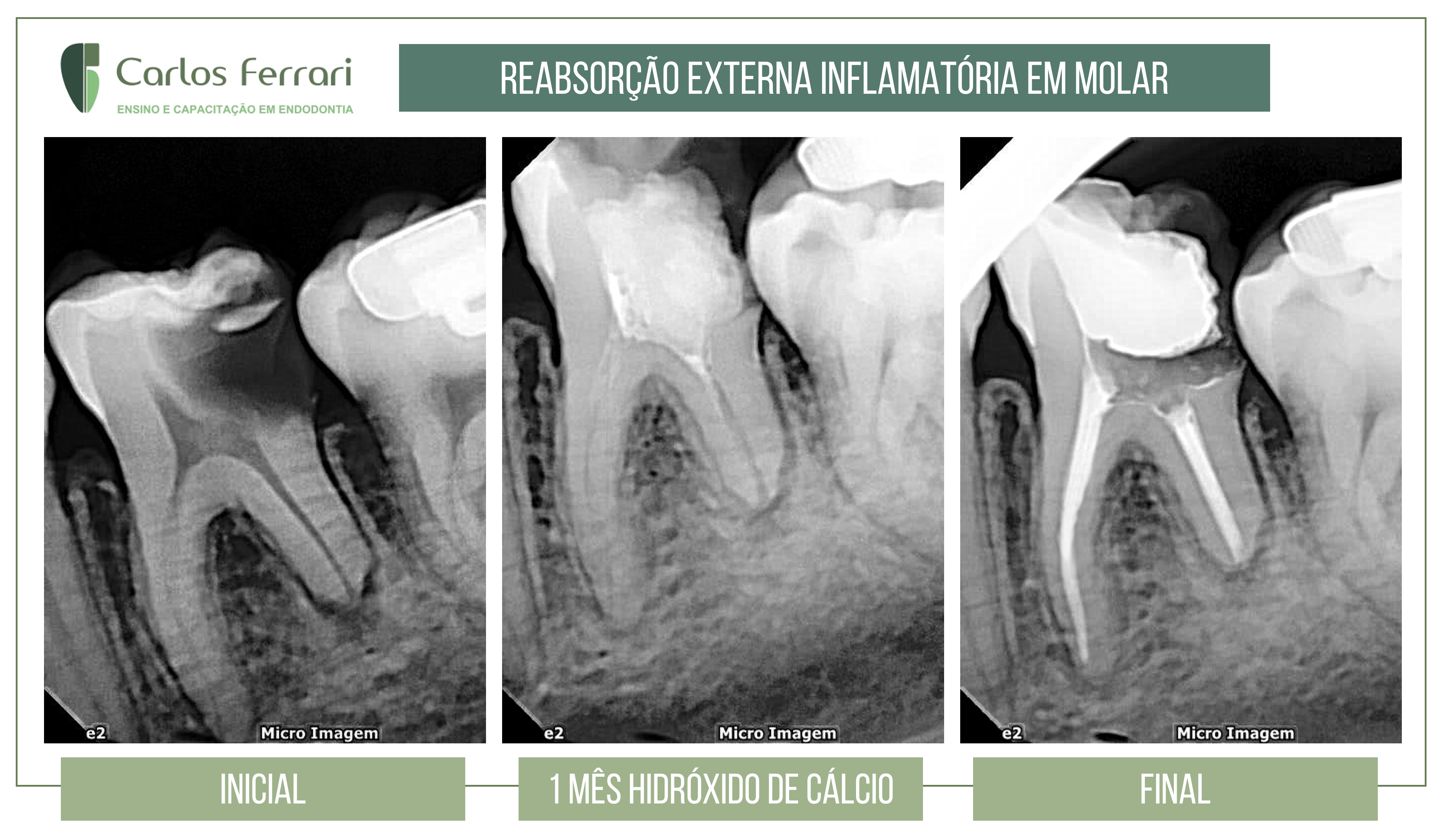
Root resorption, clinical case.
Patient sought restorative treatment and was referred for endodontic therapy. There was no painful symptomatology. On clinical examination, extensive caries and absence of response to vitality test. Radiographic examination showed an image compatible with external inflammatory resorption. After decontamination and preparation of the canals and medication with calcium hydroxide for 1 month the filling was performed.
Case conducted by student Jéssica Dias from class V of the Specialization in Endodontics at HPG Brasília.
In: Machado, Ricardo. Endodontics: Biological and Technical Principles. Available at: GEN Group, GEN Group, 2022.]
Introduction
Tooth loss due to caries or periodontal disease has decreased significantly, mainly due to prevention strategies and programs.1 However, other reasons may lead to edentulism, such as genetic and hormonal changes, systemic involvement (associated or not with the use of medications), and tooth resorption.2-7 2-7 These are caused by the action of clastic cells that lead to progressive or transient loss of cementum or cementum and dentin.8-11 In deciduous and permanent teeth, these are usually physiological and pathological, in that order.
Teeth affected by tooth resorption are usually asymptomatic. Therefore, the clinician must know the types, causes and mechanisms related to these pathologies for early diagnosis and correct treatment plans.
The objective of this chapter is to address relevant aspects associated with tooth resorption.
Activation and mechanisms of resorption
The alveolar bone is covered by the gingiva, is separated from the root cementum by the periodontal ligament, and undergoes constant resorption and apposition due to the action of osteoclasts (box "Additional information on osteoclasts") and osteoblasts, respectively. The epithelial remnants of Malassez present in the periodontal ligament release epidermal growth factor (EGF) to maintain osteoclasia of the inner alveolar walls, preventing ankylosis (see below). Furthermore, cementoblasts do not have specific receptors for the chemical mediators of resorption. As long as the root surface is covered by cementoblasts and pre-cementum, there will be no resorptive process. The same occurs when odontoblasts and pre-dentin cover the dentin.
When a tooth is submitted to physical, chemical or biological trauma, there may be the beginning of an inflammatory process. This is followed by exudative phenomena and the production of local chemical mediators such as plasmin, which acts on osteoblasts and promotes the release of collagenase, which is responsible for the degradation of osteoid tissue. At the same time, prostaglandin E2 interacts with osteoblast surface receptors and induces cytoskeletal contraction, promoting the exposure of small areas of mineralized tissue. Clasts are attracted, adhere to these areas by means of their folded edges, and start the resorptive process. Organic and inorganic fragments are phagocytized, processed inside these cells, and later released to the environment. Therefore, tooth resorption occurs from the interaction between chemical mediators (box "Main chemical mediators involved in the stimulation of clastic cells and maintenance of resorption") and constituents of the basic multicellular unit (BMU) - blasts, macrophages and clasts.
https://ferrariendodontia.com.br/wp-admin/post.php?post=2075&action=edit