Root resorption.
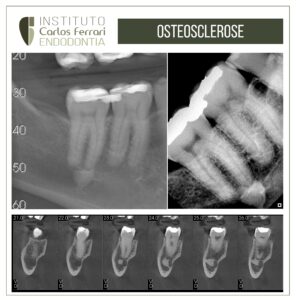
Patient sought care complaining of pain and swelling in the gingiva by palatine. On clinical examination, it was observed gingival edema and periodontal probing of 9mm depth in the region. Palpation and percussion tests were negative and vitality was positive, with a more exacerbated response in relation to the other teeth, therefore, as a pulp diagnosis, asymptomatic irreversible pulp inflammation. Radiographic and tomographic examination revealed images compatible with external cervical resorption.
The proposed treatment for root resorption was endodontic and surgical with restoration of the resorbed area by intentional reimplantation.
Root resorption In Ricardo Machado: Endodontics. Biological and Technical Principles. Ed. Gen, 2022:
Invasive cervical external tooth resorption. It starts at the cementoenamel junction after internal and/or external whitening, trauma, surgical procedures, periodontal and/or orthodontic treatments. Their etiology is still not completely elucidated, but trauma is frequently associated with their occurrence. The most affected teeth are: upper canines and incisors, and lower molars (vital, necrotic, or endodontically treated). In vital teeth, initially, there is no pulp involvement, because the pathological process originates in the periodontal ligament. Microorganisms and their by-products present in the gingival sulcus trigger an inflammatory reaction. Consequently, there is a release of chemical mediators responsible for resorption (cytokines and prostaglandins), which advance in the coronal and apical direction.
Over time, pulp necrosis may occur, but usually the resorption bypasses the pulp cavity without contacting it directly. Heithersay (1999) proposed a classification for invasive cervical external tooth resorption considering its evolution. Invasive cervical external tooth resorption expands first in a coronal direction and then apically. In the early stages, the pulp remains healthy due to the presence of pre-dentin. In older resorptions (Class IV), there may be communication with the pulp cavity. Additional resorption pathways are also created reaching the apical periodontal ligament. The root structure is gradually compromised, assuming a beehive appearance. Clinically, a pinkish spot can be observed in the cervical region near the gingival sulcus. In other cases, the tooth does not present perceptible changes. When vitality is present, the responses to thermal tests are within normal standards. In cases of necrosis or in teeth already treated endodontically, these responses are negative.
During periodontal probing, significant bleeding is usually observed due to the presence of granulation tissue. The edges of the resorbed surfaces are sharp, thin and brittle. Radiographically, the most recent lesions are radiolucent and the older ones have an osteoid aspect (radiolucent areas with radiopaque dots). Invasive cervical external Class I and II and Class III and IV resorptions resemble carious lesions and internal resorptions, respectively. However, in external resorptions, the contour of the root canal remains visible due to the integrity of the pre-dentin layer.