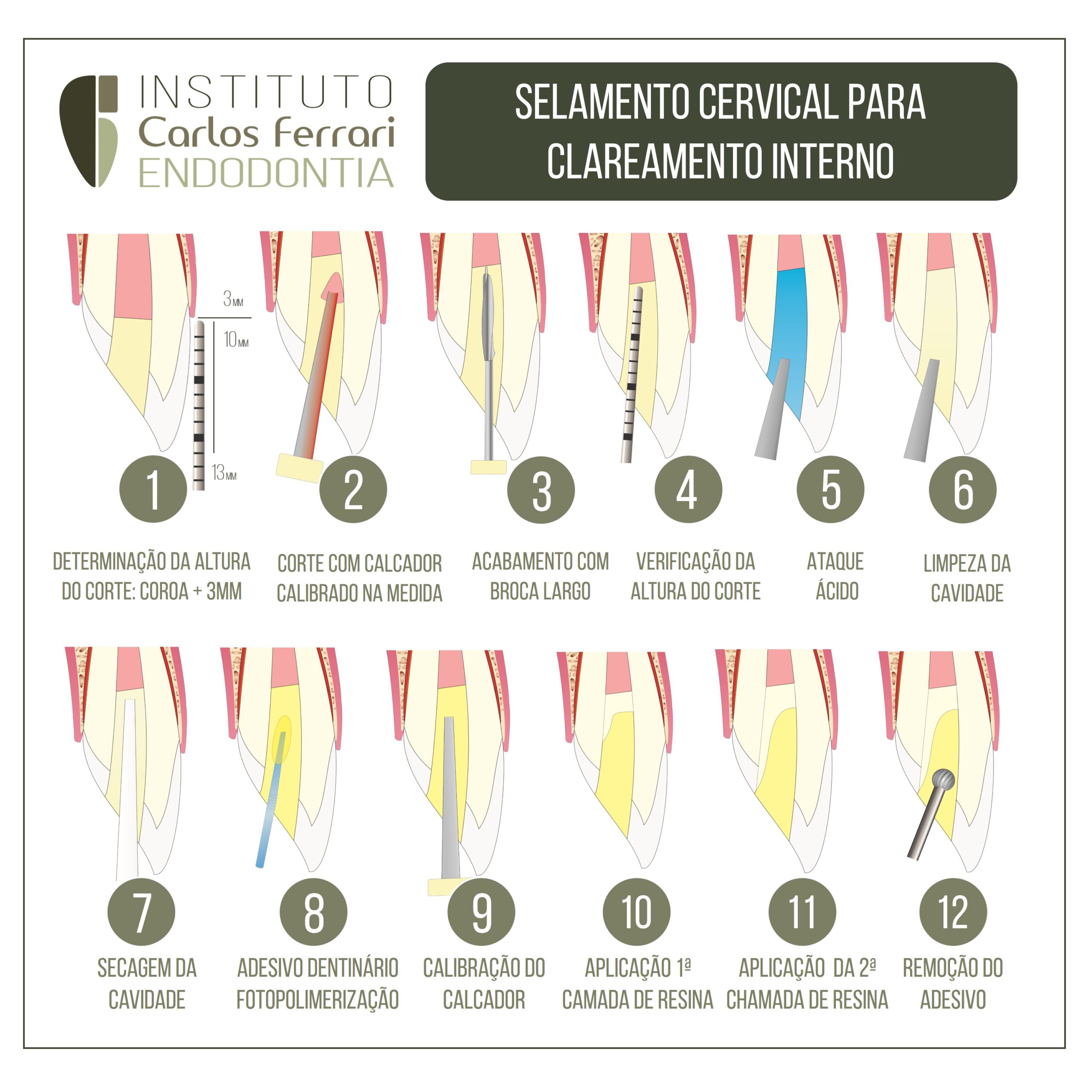
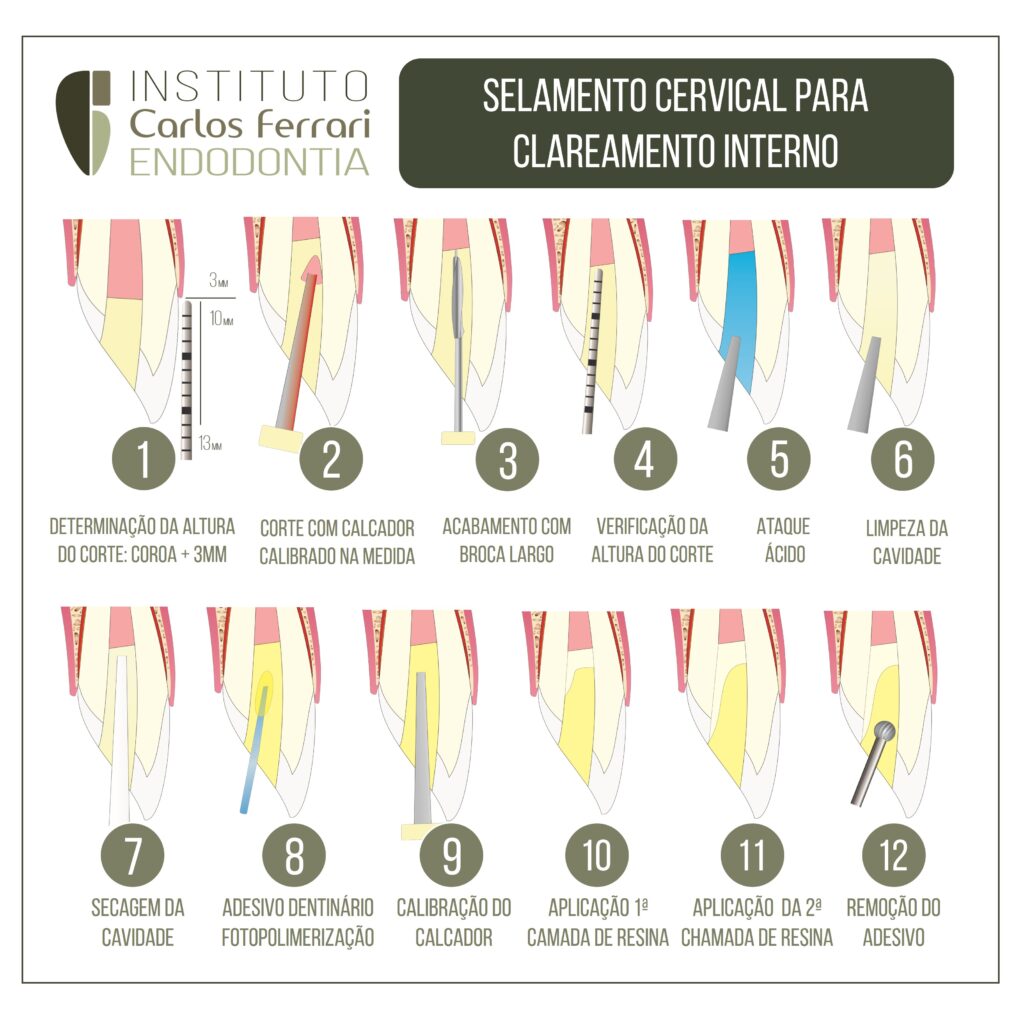
Selamento cervical para clareamento interno. Selamento prévio à realização de clareamento dental interno, medida obrigatória para prevenção da reabsorção cervicar inflamatória, sequela possível de acordo com a literatura.
In: Costa et al. Comparação de dois tipos de tampão cervical durante clareamento dental interno. Rev APCD 2010.
INTRODUÇÃO
O clareamento de dentes desvitalizados tem se tornado um procedimento comum na prática odontológica, principalmente
em dentes anteriores escurecidos. Dentre as principais causas referentes à alteração da cor em dentes desvitalizados pode-se citar a presença de polpa necrótica, hemorragia intrapulpar, medicamento de uso intracanal, trauma e material de obturação do canal radicular.
O clareamento de dentes desvitalizados foi proposto em 1924 através do uso de uma solução saturada de perborato de sódio e
peróxido de hidrogênio2 , sendo que tal produto ainda é utilizado até os dias de hoje. Tal técnica apresenta resultados esteticamente satisfatórios, mas não é raro deparar-se com um efeito colateral indesejado – a reabsorção cervical externa -, que pode prejudicar ou até mesmo inviabilizar a permanência do elemento dental na cavidade bucal.
A etiologia nestes casos tem sido dada por uma reação inflamatória gerada no ligamento periodontal, resultando na ação osteoclástica potencializada por defeitos no cemento, no entanto a causa desta resposta inflamatória não é bem elucidada, acreditase que há uma íntima ligação com a ação cáustica do peróxido de hidrogênio levando à denaturação de dentina e consequentemente à resposta imunológica.
Estudos que avaliaram diferentes agentes clareadores mostraram que todos apresentam efeito citotóxico e genotóxico
quando aplicados em cultura de fibroblastos5, onde peróxido de hidrogênio mesmo quando misturado ao perborato de sódio resultou em grandes efeitos citotóxicos quando exposta a células de ligamento periodontal.
Além disso, é possível o aumento de permeabilidade dentinária com o uso de tais substâncias, facilitando a passagem substancial do mesmo à região periodontal, fato observado na avaliação da difusibilidade do agente clareador da câmara pulpar à região
externa do dente, que é potencializado e proporcional à concentração de peróxido de hidrogênio.
Assim, uma barreira cervical durante o clareamento dental interno tem sido proposta para minimizar este efeito adverso. O
primeiro material a ser utilizado com esta finalidade foi o cimento de policarboxilato em 1983, desde então, diversos materiais têm sido analisados na busca daquele que promova o melhor vedamento, porém, o índice de infiltração ainda é grande. O Cimento de Ionômero de Vidro tem sido amplamente utilizado na clínica odontológica como materiais forradores, cimentantes e restauradores, além de liberar flúor, possui capacidadede aderir quimicamente ao tecido dental, e seu coeficiente de expansão térmica é semelhante ao da estrutura dentária. No entanto, trabalhos têm demonstrado que o ionômero de vidro convencional apresenta baixa capacidade de vedamento periférico, e quando o mesmo é modificado por adição de monômeros resinosos, torna-se mais eficaz em restaurações resultando em menores microinfiltrações. á os cimentos resinosos são materiais compostos, constituídos de uma matriz de resina, utilizados na cimentação de restaurações indiretas de resina composta. Em comparações
com o ionômero de vidro, o cimento resinoso dual tem apresentado resultados superiores em relação a microinfiltração
das peças cimentadas.