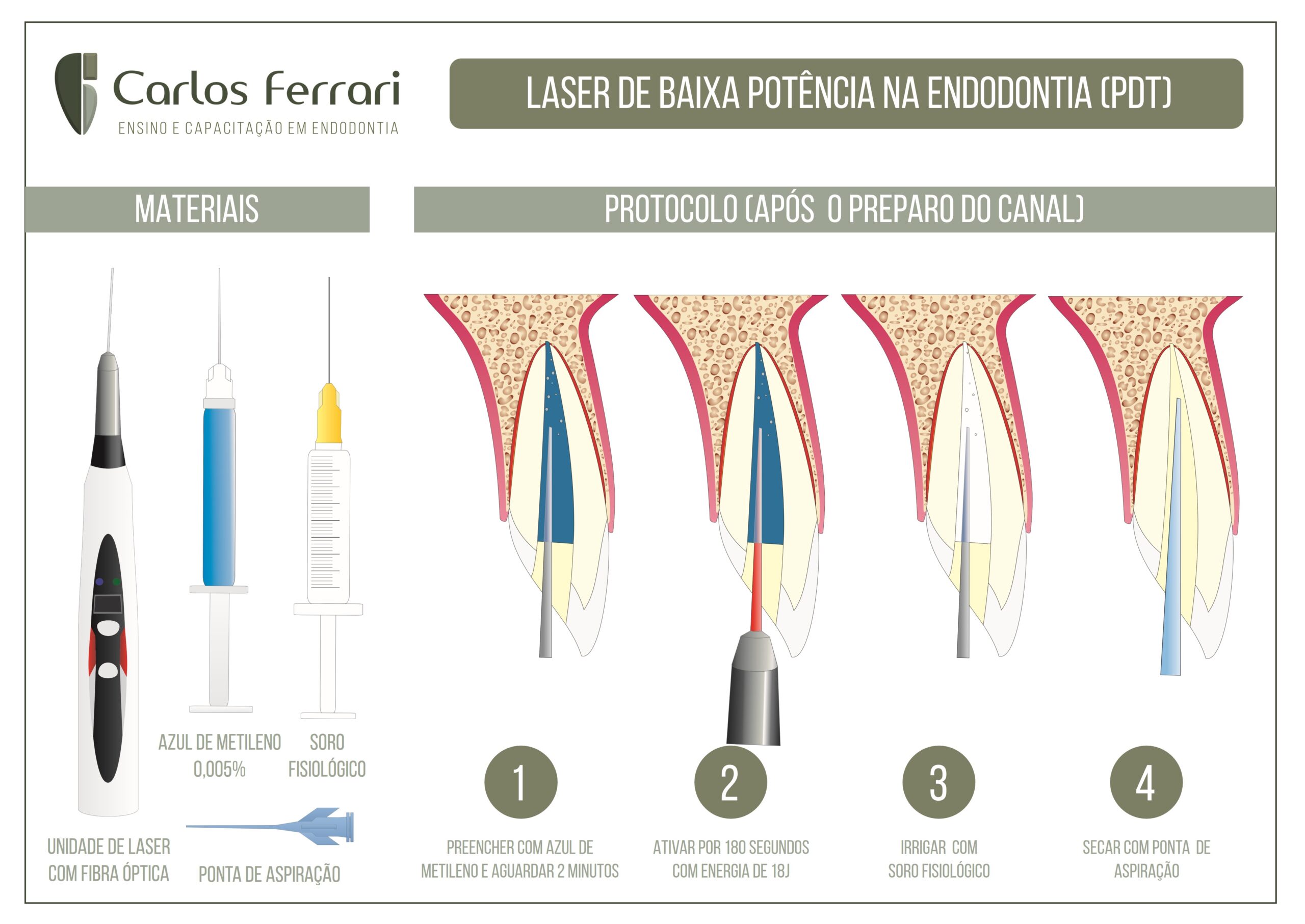
Photodynamic therapy in endodontics, using lasers, especially low power lasers, is already a reality in most offices, especially for photodynamic therapy. Below is a guide to the materials used and the protocol for using this important technology in endodontic treatment.
In: Ricardo Machado. Endodontics. Biological and Technical Principles. Editora Gen, 2022.
Introduction
The basic goal of endodontic treatment is to maintain or restore the health of periapical tissues by cleaning and filling the root canal system. The biomechanical preparation and intracanal medication (when used) are responsible for disinfection. The obturation maintains the obtained cleanliness, and is essential for the long-term success of the treatment.
Studies have shown limitations of biomechanical preparation and intracanal medication in reducing the microbial contingent present in the root canal system.
Complementary strategies have been proposed to enhance disinfection of the root canal system, such as irrigant agitation, ozone therapy, and photodynamic therapy.
Photodynamic therapy is based on the use of a non-toxic photosensitive dye irradiated by a visible light of adequate wavelength in the presence of oxygen. It is also called antimicrobial photodynamic therapy, light-activated disinfection, antimicrobial photodynamic chemotherapy, and photoactivated disinfection. This strategy has shown good results in eliminating remaining microorganisms after biomechanical preparation, with or without the use of intracanal medication.
The objective of this chapter is to expose the use of photodynamic therapy as an auxiliary strategy to clean and disinfect the root canal system.
History
Using light to restore health is an ancient practice. Early civilizations in Egypt, India, and China sought to treat diseases such as psoriasis, vitiligo, and cancer by means of sunlight.
The first reports that the association between dyes and light could generate antimicrobial effects date back more than 100 years. In 1900, Oscar Raab and Hermann von Tappeiner observed that red acridine could absorb ambient light and have toxic effects on protozoan cultures. Von Tappeiner and Jesionek (1903) found that it was possible to treat skin cancer lesions using topical eosin activated by white light. A year later, Von Tappeiner and Jodlbauer (1904) demonstrated that the presence of oxygen was paramount for the photosensitization process to occur.
More structured research on photodynamic therapy was initially developed in the medical field.38-43 Over time, this strategy has also been studied in dentistry, and more specifically in endodontics.
In recent years, in vitro and in vivo research has shown that photodynamic therapy can be an important auxiliary strategy in the process of cleaning and disinfecting root canals.
Mechanism of action
The mechanism of action of photodynamic therapy occurs when the dye (photosensitizing agent) absorbs photons from light, and its electrons pass to an excited state - triplet state. In the presence of a substrate (oxygen), when it returns to its fundamental state, the photosensitizing agent transfers energy to the substrate, forming free radicals of high cytotoxicity.
Two mechanisms (reactions) explain how the photosensitizer in the triplet state can react with biomolecules. The type I reaction involves the transfer of electrons to substrate molecules. This leads to the production of free radicals that react rapidly with oxygen, resulting in the production of superoxides, hydroxyl radicals, and hydrogen peroxide.
In the type II reaction, the excited photosensitizer transfers energy to oxygen, leading to the production of electronically excited molecules - singletet oxygen. Superoxides, hydroxyl radicals, hydrogen peroxide, and singlet oxygen cause damage to the cell membrane, mitochondria, nucleus, and other microbial cellular components.
It is difficult to distinguish between the two reactions, however, type II is accepted as the main route of microbial cell destruction during the performance of photodynamic therapy.
Photodynamic therapy in endodontics.