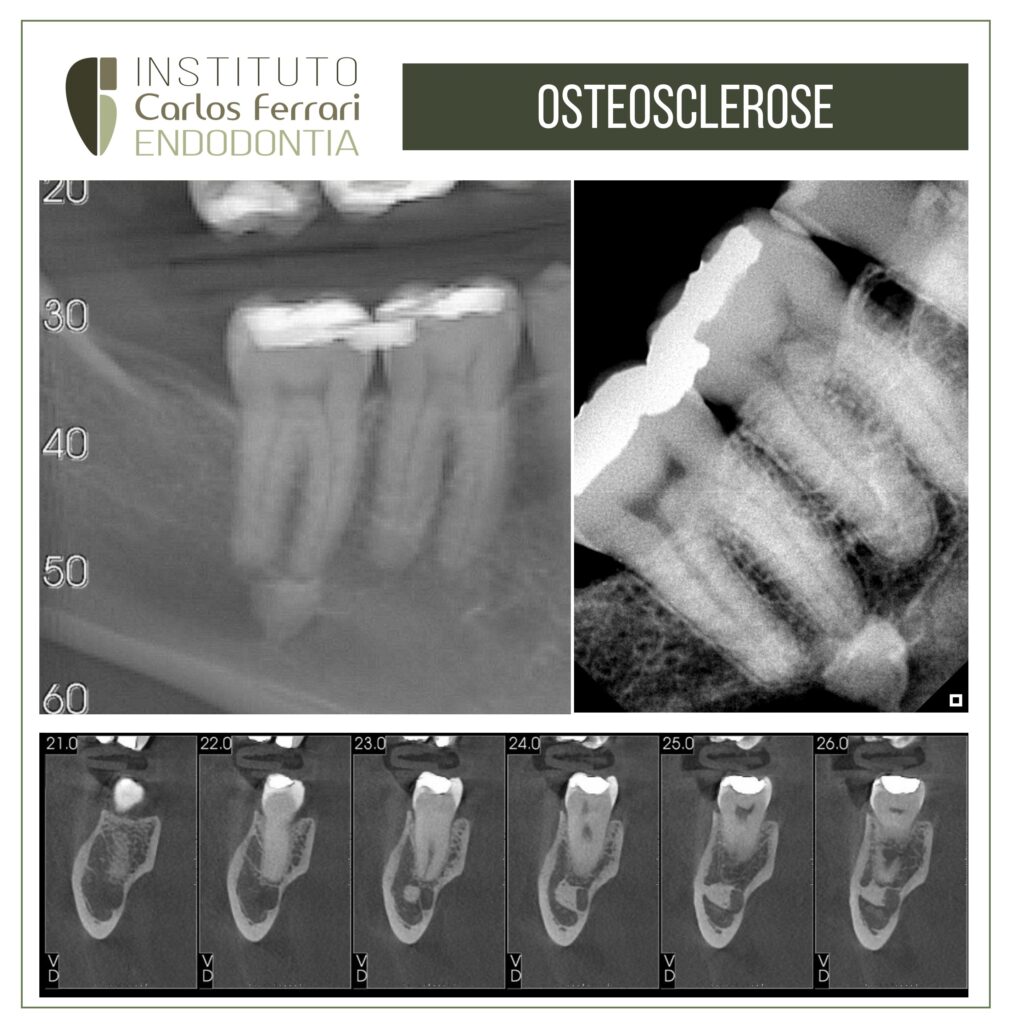
Osteosclerosis in the apical region.
Patient sought care reporting pain on chewing in the lower right region.
All the tests on teeth 44 to 47 were negative, and the pulp was normal. Radiographic examination revealed a circumscribed radiopaque image in the apical region of the mesial root of tooth 47. A CT scan revealed that the hyperdense image does not communicate with the periapex and is contiguous with the mandibular canal, and therefore corresponds to osteosclerosis.
Occlusal adjustment was carried out and the patient was advised to continue.
Case carried out by colleague Mariana Sanches, a former endodontics specialization student at HPG Brasília.
Osteosclerosis: in Silva, Afonso Manuel de Castro. "Idiopathic osteosclerosis: a radiographic study of its prevalence in a Portuguese population." (2006).
Osteosclerosis is a generic term used to describe a thickening of the bone
which becomes compact, with narrowing of the medullary spaces
and increased radiopacity. Routine radiographic examinations of the jaws often show asymptomatic osteosclerotic
areas, which are usually solitary but can also be multiple
and bilateral.
When the etiology of the radiopacity can be determined, as in inflammatory radiopaque apical
lesions, it would be more appropriate to use a more
specific nomenclature, in this case, condensing osteitis (CO). On the other hand, when no apparent cause can be attributed to the osteosclerotic area
, the term idiopathic osteosclerosis
(OI)8 is used. This image, originally described by Stieda in 1905 apud Greenspan (1995) and
Caballes (2004)14, translates into the existence of a localized region of abnormally dense
medullary bone, unrelated to the existence of any infection, disease
systemic or neoplastic. Its shape can be rounded, elliptical or irregular, and
its size can vary from a few millimeters to one to two centimeters in diameter.
Regardless of its size, it is confined to the limits of the bone and does not cause expansion
of the cortical bone.
The radiopacity is variable in size, shape, contour and density,
and may be associated with the roots of vital teeth or be completely separated from them
by normal trabecular bone. Its contour is usually distinct, and its area can be
uniformly radiopaque or with a diffuse appearance with radiolucent stippling. When located in edentulous areas, it can represent areas of OC that persist after the removal of the teeth involved, or be the result of trauma
surgical or delayed healing.
From a
histological point of view, it consists of dense, trabeculated, non-inflammatory vital bone. It is not
classified as a benign neoplasm because, unlike the latter, it does not continue to grow until it is
treated. It is classified by Matteson
as a hamartoma, i.e. an atypical
development of normal tissue caused by abnormal growth and development.
hamartomas are not considered true neoplasms because they do not grow
indefinitely.
Although it is often referred to in the literature as OI on the basis of
its unknown etiology, it is also frequently referred to as an island of dense
bone. The literature has also found various other names for this
lesion: enostosis, sclerotic bone, compact bone island, bone scar, ebony,
Introduction
Periapical focal osteopetrosis, endosteoma. This variety of terminology denotes the
confusion that exists in the classification of focal osteosclerotic lesions. In fact, the term
enostosis is used in the literature in a somewhat confusing way, since for some
authors it is considered synonymous with OI and for others as a type of OI
that refers to localized formations of compact bone that grow from the inner surface of
cortical bone into cancellous bone. They are the internal equivalent of exostoses, whose appearance
radiographically and histologically is similar to OI.
It is important to note that OI is not an exclusive lesion of the jaws, and can occur
in any bone of the skeleton, although it is more frequent in the bones of the
axial skeleton, particularly the pelvis, spine, ribs, femur and humerus. In 1983,
Resnick and his colleagues (et al.) investigated the existence of OI in the vertebral column of
100 cadavers aged between 46 and 93 years (average 68 years).
They removed the thoracic and lumbar vertebral bodies and radiographed them, detecting the
presence of OI in 14 % of the cadavers they examined.
OI lesions can usually be diagnosed on the basis of their
clinical and radiographic characteristics. They are easily differentiated from other more significant bone
lesions, such as bone metastases, although occasionally their
large size, growth potential and scintigraphic activity
can make diagnosis difficult. Biopsy can be used to detect histological
characteristics of lamellar compact bone, but this is a procedure that is rarely
required.
Its clinical importance is not determined by its symptoms, nor
by the complications that may arise from it, but rather by the need
to know about this entity in order to avoid unnecessary investigations or treatments
resulting from an incorrect diagnosis36. For this reason, they are referred to in the
scientific literature as "don't touch lesions", i.e. lesions that shouldn't be treated or touched,
only diagnosed and controlled.
On the other hand, possible
associations have been established between sclerotic lesions in the jaws and other systemic pathologies, such as
Gardner's syndrome, familial adenomatous polyposis, adenocarcinoma of the
intestine, chronic kidney disease and hyperparathyroidism.