Sinusite odontogênica bilateral. Caso de sinusite com origem odontológica em paciente que passou por diversos tratamentos médicos.
Paciente relatou ter passado por dois médicos otorrinolaringologistas, relatando sintomas típicos de sinusite, dor e pressão na região do seio maxilar, sendo submetido a tratamentos diversos, sem melhora a longo prazo.
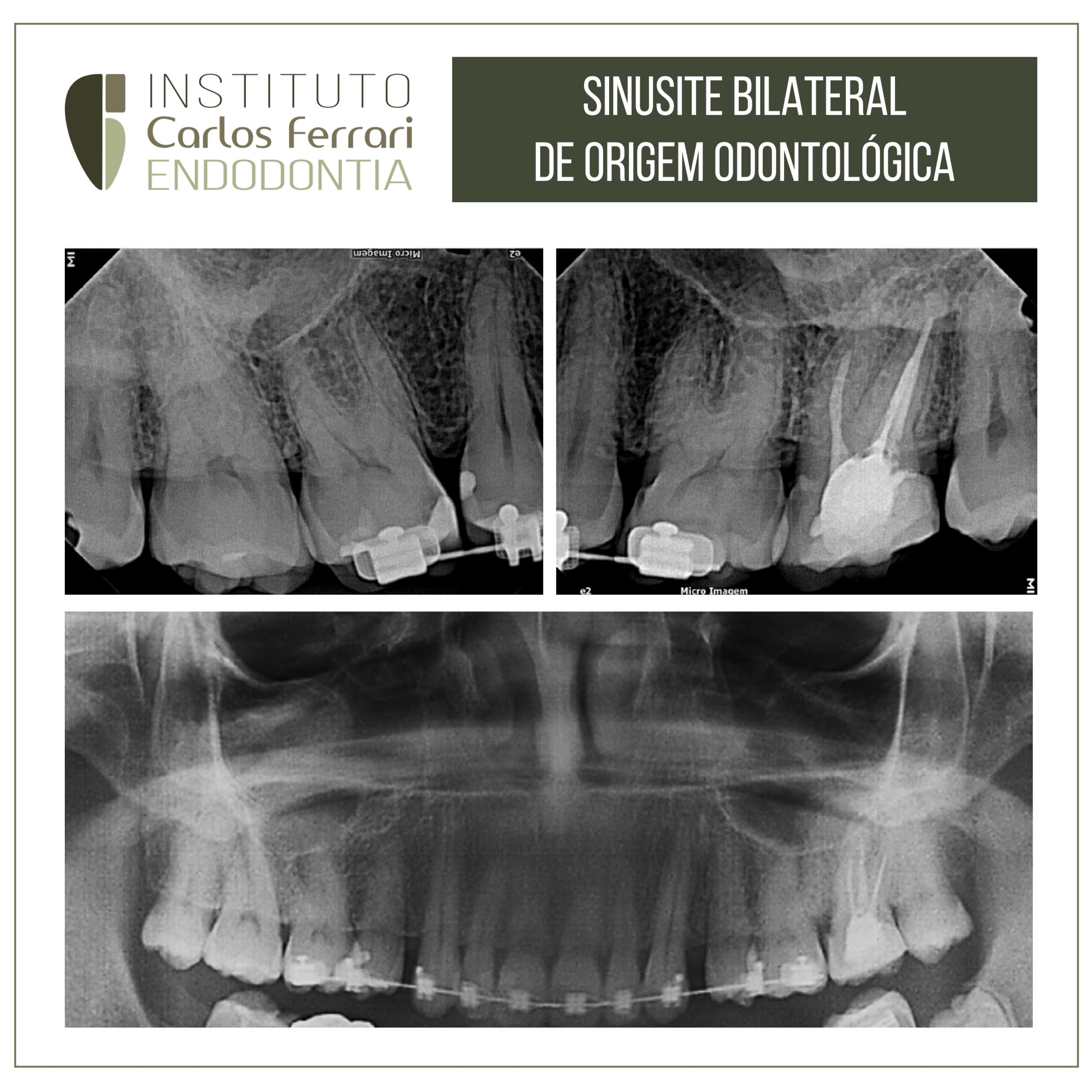
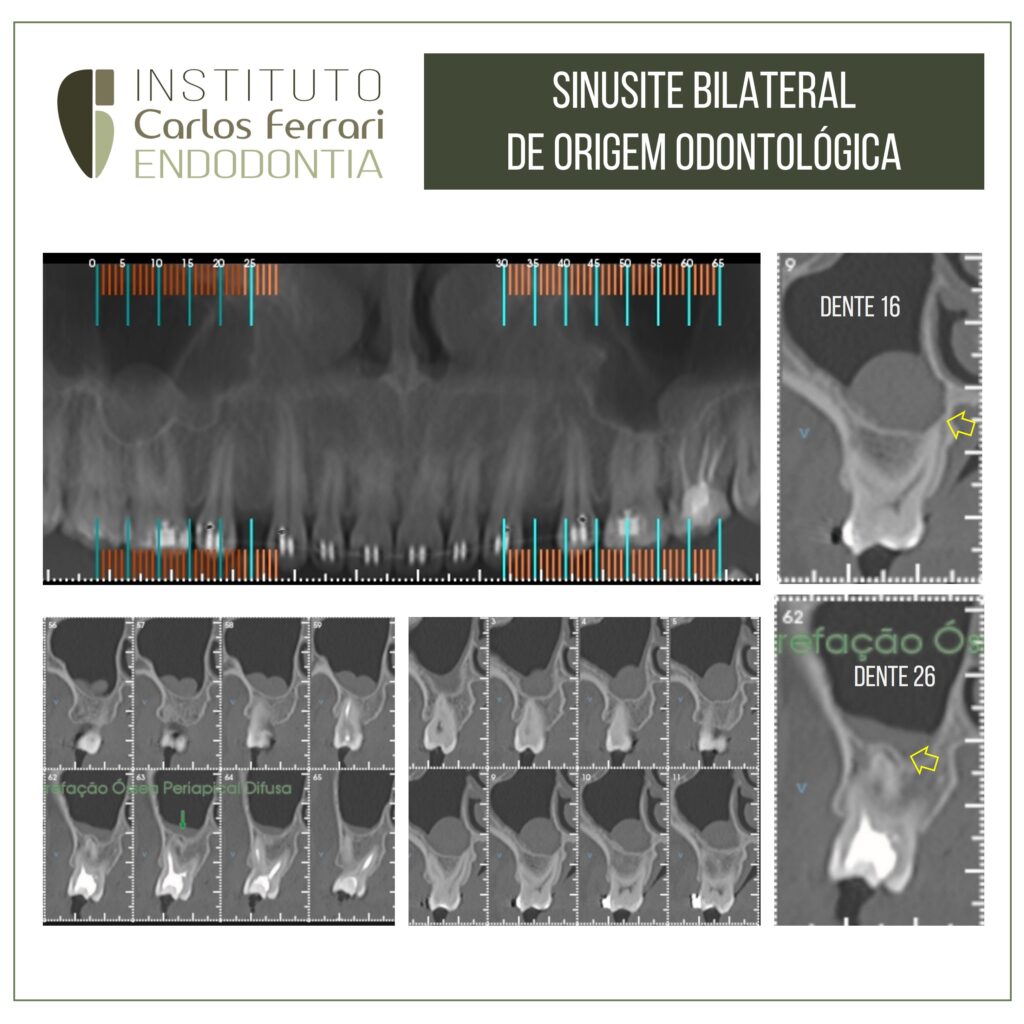
Ao exame clínico, os dentes 16 e 26 não apresentaram vitalidade positiva, sendo que o dente 26 apresentou dor à palpação e percussão. A radiografia panorâmica e a periapical revelaram tratamento endodôntico realizado no dente 27 e não forneceram imagens conclusivas sobre a relação entre sinusite e infecção endodôntica. O exame tomográfico revelou imagens de rompimento de cortical do seio maxilar e espessamento da mucosa sinusal em torno dos ápices.
Diagnóstico: sinusite de origem odontológica ou síndrome endo-antral, bilateral, causada por periodontite apical nos dentes 16 e 27. Os dentes foram tratados endodonticamente e houve remissão dos sintomas.

In: Gonçalves et al. Sinusite de Origem Odontológica. Relato de caso. SEMINÁRIO TRANSDISCIPLINAR DA SAÚDE – nº 04 – ano 2016
INTRODUÇÃO
O crânio possui cinco cavidades pneumáticas, denominadas de seios (etmoidal, esfenoidal, frontal e maxilar). O seio maxilar é o maior deles, se forma na vida intrauterina através da invaginação da cavidade nasal, e continua sua formação posteriormente, sendo responsável pela umidificação e aquecimento do ar inspirado e funciona como caixa de ressonância para a voz (Peterson et al., 2005; Brook, 2006; Scuderi et al., 1993).
A sinusite odontogênica (ou sinusite maxilar) situa-se no seio maxilar, onde ocorre uma inflamação da membrana. Didaticamente, divide-se de duas formas: 1) traumática (que envolve impacto direto na região, afetando o soalho do seio) e 2) não-traumática.
Várias causas estão associadas à esta última como: infecções gerais do organismo citando os resfriados, pneumonia,
gripe, entre outras; bem como as causas odontogênicas, proveniente de focos infecciosos próximos ao seio, destacando a doença cárie, iatrogenias, cistos odontogênicos e doença periodontal (Mehra et al., 1999; Maia-Filho et al., 2007).
Clinicamente, podemos dividir a sinusite odontogênica em aguda ou crônica. A primeira baseiase na dor intensa irradiada para o hemiarco, dor periodontal, dor à percussão e/ou pressão, cornetos edemaciados, secreções nasais purulentas e fístula oroantral. A segunda, tem-se fraca sintomatologia podendo apresentar cefaléia, sensação de pressão, e ainda quadros agudos (Horch, 1995).
Muitas vezes as raízes dos dentes pré-molares e molares ficam em íntimo contato com o seio pois estão logo abaixo do soalho, e qualquer acometimento nessa região pode drenar para o seio maxilar, desencadeando a sinusite de origem odontogênica na membrana de Schneider representada pela reação inflamatória e/ou infecciosa. (Mehra & Murad, 2004; Brook, 2006; Costa et al., 2007).
A microbiologia existente nas infecções dentro seio é constituída por uma flora polimicrobiana, composta por bactérias aeróbias e anaeróbias (Peterson et al., 2005), as quais as anaeróbias são provenientes da orofaringe, infecção periodontal e endodôntica.
Quanto ás aeróbias, estão em menor número. Todavia, ambos agentes bacterianos estão presentes nas duas apresentações de sinusite, aguda e crônica (Brook, 2005).
O processo diagnóstico inclui investigar a história clínica da maneira detalhada, realizar exame físico (extra e intrabucal) completo e obter exames de imagens, tais como radiografias intrabucais (periapical) e extrabucais (panorâmica e tomografia) (Vale et al., 2010). Esta última, é a mais preconizada em virtude de sua alta qualidade, menor exposição à radiação e elevada capacidade em avaliar a anatomia sinusal, permitindo observar lesões na mucosa, suas extensões e variações anatômicas, e estruturas ósseas em várias perspectivas (Nishimura e Ilzuka, 2002).
O tratamento consiste em eliminar os fatores causais e a infecção presente no seio (Brook, 2006). Normalmente combina-se as terapêuticas: farmacológica e cirúrgica para solucionar tal patologia (Costa et al., 2007; Vale et al., 2010), pois a administração de antibióticos é essencial no processo terapêutico prevenindo complicações, destacando a penicilina, devido ao seu amplo
espectro (Mathew et al., 2012; Sanchéz et al., 2011). A utilização de descongestionantes nasais e gotas de hidratação também ajudam nesse processo (Harvey et al., 2007).
Sinusite odontogênica bilateral