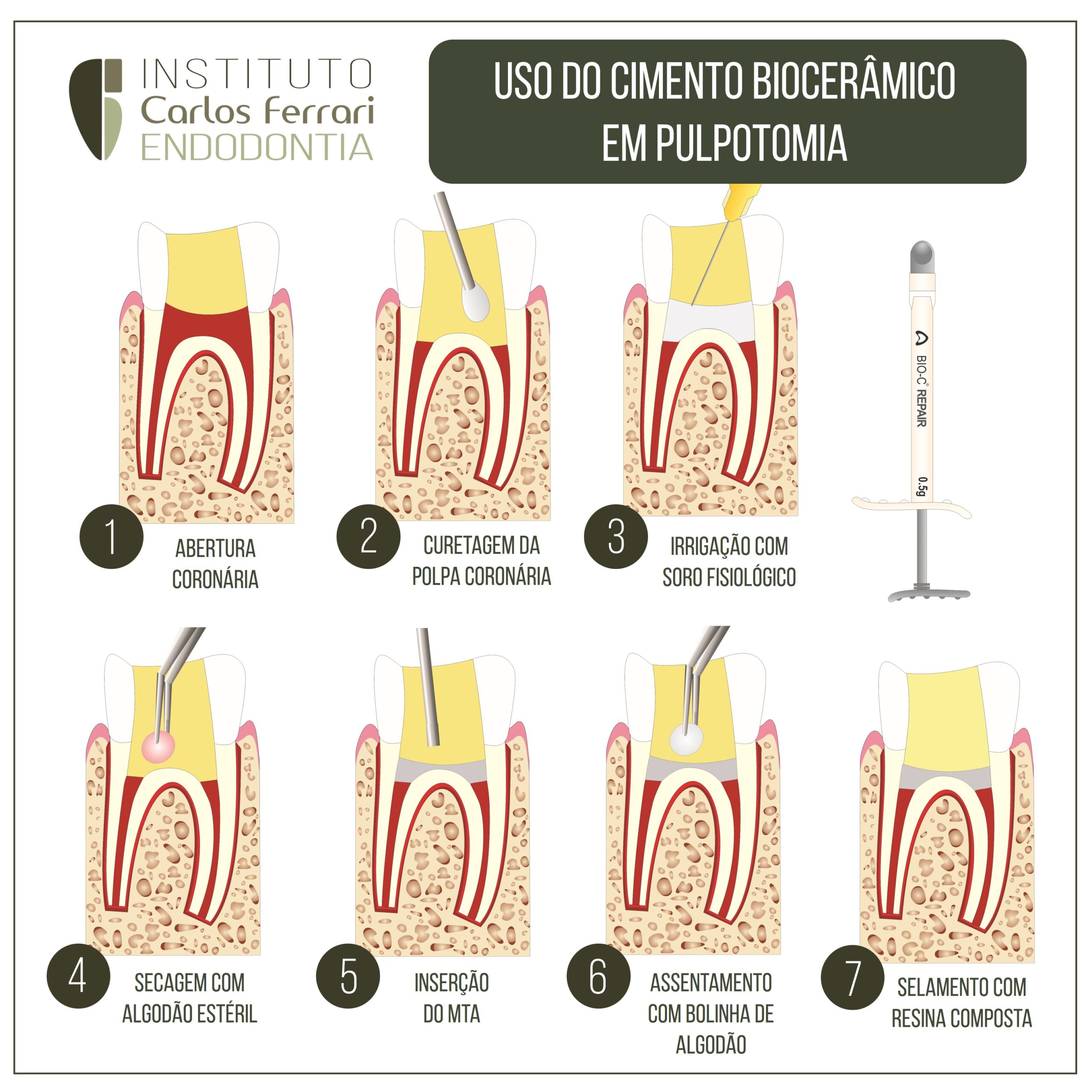
Cimentos biocerâmicos em pulpotomia. O MTA e os cimentos biocerâmicos de reparação em geral, são o padrão ouro para a pulpotomia no tratamento de dentes com vitalidade pulpar e rizogênese incompleta.
A seguir um roteiro básico de utilização do material, recomendado em nossos cursos de pós graduação em endodontia.
In: Santos & Machado. Pulpotomia em dentes permanentes. UNIUBE,2019.
- INTRODUÇÃO
A polpa dentária é um tecido frouxo, vascularizado, localizado no interior das
paredes da dentina. Este tecido desempenha um papel muito importante na
longevidade do dente, cujas funções são: formativa, sensitiva, nutritiva e defensiva.
A exposição da polpa pode ser causada por diversos fatores, como cárie, fratura,
fendas ou uma margem de restauração aberta, o que causará a inflamação do
tecido pulpar, podendo resultar em necrose, caso não seja feita a intervenção
brevemente (SOLOMON et al., 2015).
É importante ressaltar que estudos vêm sendo realizados nestes casos e
uma das propostas de intervenção é a pulpotomia, que, nada mais é, que a remoção
parcial ou total da polpa coronária, a qual sofreu alterações patológicas reversíveis
ou irreversíveis, mantendo, assim, a vitalidade do restante do remanescente
dentário. O benefício de manter a vitalidade da polpa é extremamente importante,
uma vez que mantém todas as funcionalidades de propriocepção do dente (ZANINI;
HENNEGUIN; COUSSON, 2016).
Há controvérsias em relação à eficácia da pulpotomia, como tratamento em
dentes permanentes, tendo em vista que, na maioria dos casos, esse tipo de
tratamento é indicado para dentes decíduos ou molares permanentes sem
apicificação. Entretanto, estudos recentes demonstraram taxas de sucessos, quando
realizado em dentes permanentes (KUMAR et al., 2016).
O sucesso por trás dos procedimentos de pulpotomia é baseado em
diversos fatores, como a capacidade de reestruturação da polpa radicular restante,
remoção de todo tecido pulpar infectado e colocação de um medicamento adequado
para o tratamento a ser feito. Ao realizar a escolha do medicamento a ser utilizado, é
importante observar a sua biocompatibilidade, capacidade de vedação e atividade
antimicrobiana, quando este é colocado em contato com a polpa inflamada
(SOLOMON et al., 2015).
Estudos realizados demonstram que o Hidróxido de Cálcio e o Trióxido
Mineral Agregado têm sido os medicamentos utilizados com mais eficácia neste tipo
de tratamento. O Hidróxido de Cálcio apresenta resultados positivos, porém, devido
às suas restrições, vêm caindo em desuso na pulpotomia nos últimos anos (TAHA;
AHMAD; GHANIM, 2017).
O Hidróxido de Cálcio tem propriedades bactericidas e grande capacidade
de formação de tecido mineralizado nos dentes humanos, mas, estudos apresentam
várias desvantagens, como fraca adesão a dentina, capacidade de vedação
deficiente, formação de ponte de dentina imprevisível e presença de defeitos, que
podem atuar como vias de infiltrações (NOSRAT; PEIMANI; ASGARY, 2013).
Por outro lado, o MTA (Agregado Trióxido Mineral) vem sendo muito
utilizado, obtendo estudos favoráveis, desde que foi introduzido na endodontia.
Devido às suas vantagens em relação aos outros materiais utilizados, por exemplo,
tem uma excelente adaptação marginal, induz a proliferação de células,
biocompatibilidade, além de uma boa formação de ponte de dentina, nos casos de
capeamento direto e pulpotomia (BARNGKGEI; HALBOUB; ALBONI, 2013).
Atualmente o MTA (Agregado Trióxido Mineral) é considerado o material
ideal para o tratamento de polpa vital em dentes permanentes, mas é relatado por
alguns profissionais dificuldade no manuseio e mistura do MTA (Agregado Trióxido
Mineral) e descoloração dental após o tratamento. Consequentemente, materiais a
base de silicato de cálcio mais recentes por exemplo o Biodentine, possui as
propriedades do MTA original, mas com uma manipulação mais fácil e sem
descoloração. O biodentine várias vantagens incluindo boa capacidade de vedação
resistência a compressão adequada e um relativo curto tempo de presa inicial
(TAHA, 2018).
De acordo com estudos apresentados, a pulpotomia surge como uma opção
de tratamento para dentes permanentes, com pulpite irreversível, tendo uma taxa de
sucesso clínico, a médio prazo, aceitável. No entanto, a taxa de eficácia, a longo
prazo, permanece questionável, dependendo de diversos fatores que envolve o
tratamento (KUMAR et al. 2016).